Table of Contents
Introduction:
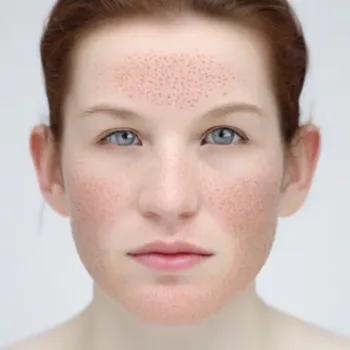
Seborrheic dermatitis is a common and chronic skin condition that affects millions of individuals worldwide. Characterized by redness, itching, and flaking, seborrheic dermatitis primarily affects areas rich in oil glands, such as the scalp, face, and chest. While it is not a serious medical condition, seborrheic dermatitis can be persistent and, at times, challenging to manage. In this comprehensive article, we will delve into the intricacies of seborrheic dermatitis, exploring its causes, and symptoms, and offering a comprehensive guide to effective management strategies.
What is Seborrheic Dermatitis?
Seborrheic dermatitis is a chronic inflammatory skin condition that predominantly affects areas with a high density of sebaceous (oil) glands. The condition is characterized by red, itchy, and flaky skin, and it often occurs in areas where the skin is oily. While the exact cause is not fully understood, factors such as genetics, yeast overgrowth, and environmental factors may contribute to its development.
you can also read about Impetigo Symptoms, Causes, Treatment, and Prevention Strategies click here
Causes:
Several factors may contribute to the onset and exacerbation of seborrheic dermatitis:
- Yeast Overgrowth (Malassezia): The yeast Malassezia is a normal inhabitant of human skin. However, an overgrowth of this yeast is associated with seborrheic dermatitis. Malassezia feeds on the natural oils (sebum) produced by the skin and breaks it down into substances that can irritate the skin, triggering inflammation.
- Excessive Sebum (Oil) Production: Seborrheic dermatitis often occurs in areas where sebaceous (oil) glands are more concentrated. Excessive production of sebum can contribute to the development of the condition. Hormonal changes, which are common during adolescence, may stimulate the sebaceous glands and exacerbate symptoms.
- Genetic Predisposition: There is evidence to suggest a genetic predisposition to seborrheic dermatitis. Individuals with a family history of the condition may be more prone to developing it themselves.
- Environmental Factors: Environmental factors, such as cold and dry weather, can worsen symptoms of seborrheic dermatitis. Additionally, exposure to harsh or irritating skincare products, as well as stress and fatigue, can contribute to flare-ups.
- Neurological Factors: Certain neurological conditions may be associated with an increased risk of seborrheic dermatitis. For example, Parkinson’s disease is known to have a connection with the development of this skin condition.
- Immune System Response: An abnormal immune response is thought to play a role in seborrheic dermatitis. Inflammation is a key characteristic of the condition, and the immune system’s response to factors like Malassezia may contribute to the skin symptoms.
- Hormonal Changes: Hormonal changes, particularly those associated with puberty, menstruation, pregnancy, and menopause, can influence the activity of sebaceous glands. Fluctuations in hormones may contribute to the development or exacerbation of seborrheic dermatitis.
- Certain Medical Conditions: Medical conditions that compromise the immune system, such as HIV/AIDS, may increase the risk of seborrheic dermatitis. Conditions like obesity and metabolic syndrome have also been associated with a higher likelihood of developing the condition.
- Medications: Some medications, such as those that suppress the immune system or affect the nervous system, may increase the risk of seborrheic dermatitis. Lithium, a medication used to treat bipolar disorder, is known to be associated with this skin condition.
Symptoms:
The symptoms can vary from mild to severe and typically include:
- Redness: Inflamed areas of the skin may appear red or have a reddish tint.
- Flaky or Scaly Skin: Fine, white or yellowish scales may develop on the skin surface, often resembling dandruff.
- Itching: Persistent itching is a common symptom, contributing to discomfort.
- Greasy or Oily Appearance: While the skin may appear flaky, affected areas often retain an oily or greasy appearance.
- Involvement of Specific Areas: It commonly affects the scalp (dandruff), eyebrows, eyelids, ears, creases around the nose, and chest.
Types:
- Scalp Seborrheic Dermatitis (Dandruff): Characterized by flaky, itchy skin on the scalp, often leading to dandruff.
- Facial Seborrheic Dermatitis: Affects areas such as the eyebrows, eyelids, and creases around the nose.
- Chest and Back Seborrheic Dermatitis: Can extend to the chest and back, presenting as red, flaky patches.
- Infantile Seborrheic Dermatitis (Cradle Cap): Common in infants, particularly on the scalp, and manifests as yellow, scaly patches.
Diagnosis:
Diagnosing seborrheic dermatitis is often based on a clinical examination by a healthcare professional. In some cases, a skin biopsy may be performed to rule out other skin conditions with similar symptoms.
Treatment Strategies:
Effective management involves a combination of lifestyle adjustments, skincare practices, and, in some cases, medical interventions. Treatment strategies may include:
- Topical Antifungal Agents: Ketoconazole: An antifungal agent available in shampoos, creams, or foams, effective in reducing yeast overgrowth.
- Topical Corticosteroids: Hydrocortisone: Mild corticosteroids can help reduce inflammation and itching.
- Calcineurin Inhibitors: Tacrolimus or Pimecrolimus: These medications are used for their anti-inflammatory properties.
- Antifungal Shampoos: Medicated shampoos containing ketoconazole, selenium sulfide, or zinc pyrithione can help manage scalp symptoms.
- Coal Tar Preparations: Shampoos or creams containing coal tar can be effective in reducing inflammation and scaling.
- Proper Skincare: Gentle cleansing with mild, fragrance-free cleansers can help manage symptoms.
- Avoiding Triggers: Identifying and avoiding triggers such as stress, cold weather, or certain skincare products can prevent flare-ups.
- Moisturizers: Using non-comedogenic moisturizers can help soothe dry or flaky skin.
- Phototherapy: In some cases, exposure to natural or artificial light under medical supervision may improve symptoms.
- Oral Medications: In severe cases, oral antifungal medications or systemic corticosteroids may be prescribed.
Living with Seborrheic Dermatitis:
Living with it requires ongoing management and care. Individuals can enhance their quality of life by:
- Consistent Skincare Routine: Establishing a consistent and gentle skincare routine tailored to the individual’s skin type.
- Regular Follow-ups: Regular follow-ups with a dermatologist to monitor symptoms and adjust treatment as needed.
- Avoiding Scratching: Avoiding excessive scratching to prevent skin damage and worsening of symptoms.
- Stress Management: Incorporating stress-management techniques, such as meditation or yoga, to reduce triggers.
- Choosing Suitable Haircare Products: Selecting haircare products that are gentle and suitable for the individual’s skin type.
Complications:
While seborrheic dermatitis is generally a benign condition, complications can arise, including:
- Secondary Bacterial Infections: Scratching the affected areas can lead to bacterial infections.
- Psychosocial Impact: Persistent symptoms may impact an individual’s self-esteem and quality of life.
Conclusion:
Seborrheic dermatitis, though chronic, is a manageable skin condition with various effective treatment options. Understanding the causes, recognizing symptoms, and adopting appropriate skincare practices empower individuals to effectively manage and minimize the impact on their daily lives. Seeking professional guidance from a dermatologist ensures access to personalized treatment plans, fostering healthier skin and overall well-being.
for more information click here

2 thoughts on “Seborrheic Dermatitis Causes, Symptoms, and Comprehensive Management”